Abstract
Background: Acute pain, the most prominent complication of sickle cell disease (SCD), results from vasoocclusion triggered by sickling of deoxygenated red blood cells (RBCs). A key factor influencing HbS oxygenation is the intracellular concentration of 2,3- diphosphoglycerate (2,3-DPG). 2,3-DPG, an intermediate substrate in the glycolytic pathway, decreases oxygen binding and stabilizes the deoxygenated hemoglobin. Pyruvate kinase (gene PKLR, protein PKR) is a rate-limiting enzyme in glycolysis; variants in PKLR may affect PKR activity, 2,3-DPG levels in RBCs, subsequent frequency of sickling and acute pain episodes (APE). There is thus a strong biological basis for exploring PKLR as a candidate gene affecting acute pain in SCD.
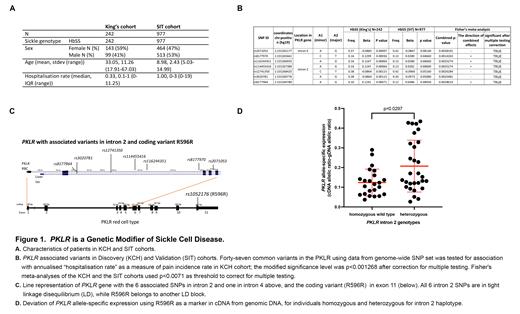
Methods: The study population for genetic association consists of 2 cohorts: 1) 242 adults with HbSS from King's College Hospital (KCH), London, UK, with complete hospitalisation records over 10 years (2004-2013 inclusive) as the "discovery" cohort; 2) 977 children with HbSS or HbSb 0 thalassemia from the Silent Infarct Transfusion (SIT) trial, with a 3-year history of severe vasoocclusive pain based on hospitalization, as the "validation" cohort. Both studies were approved by the local Institutional Review Boards at KCH and Vanderbilt University Medical Center, respectively. An independent cohort comprises 52 adults with SCD enrolled under 3 protocols - NCT00011648, NCT00081523, and NCT03685721 - approved by the NHLBI Review Board (NIH), for evaluation of imbalance in allele expression.
Genome scan for the KCH cohort was performed using llumina's Infinium "MEGA" chip (1.7m markers). The SIT DNA samples were genotyped using Illumina HumanHap650Y array 5 (661K markers) or Illumina Infinium HumanOmni1-Quad array (1.1m markers). The results were quality controlled followed by genotype imputation based on the 1000 Genomes Project phase 3 data. An annualised "hospitalisation rate" as a measure of pain incidence rate, was calculated by dividing the number of hospital admissions for severe acute pain by the number of years of observation for KCH and SIT cohorts (Fig A).
We performed association analysis with common SNPs at PKLR locus using data from our genome-wide SNP set and a linear mixed modelling approach incorporating a genetic relatedness matrix to take account of relatedness, plus sex and age as fixed covariates.
We corrected for multiple testing after quantifying the linkage disequilibrium (LD) within PKLR and used this to calculate appropriate significance levels. For the PKLR region and hospitalisation rate, the modified significance level was p<0.001268 for the discovery (KCH) cohort. For the allele expression assays, a synonymous variant, rs1052176 (R596R), in exon 11 of PKLR acted as a marker of relative expression levels of the 2 alleles of the gene. Allele specific expression was carried using the Bio-Rad digital droplet PCR system.
Results: 7 of 47 variants evaluated in PKLR were associated with hospitalization rate (LnLnHospRate) in the discovery cohort: intron 4 - rs071053, and intron 2 - rs8177970, rs116244351, rs114455416, rs12741350, rs3020781, and rs8177964). All 7 were validated in Fisher's meta-analyses of the KCH and the SIT cohorts using p<0.0071 as threshold to correct for multiple testing (Fig B). We examined the pairwise LD between PKLR variants, and found all the intron 2 variants in tight LD, while R596R belongs to another LD block (Fig C). 52 SCD individuals had the R596R variant, of which 29 were heterozygous and 23 homozygous for the intron 2 haplotype associated with APE in SCD. We performed a Wilcoxon rank sum test and compared the variation in PKLR expression between the 2 alleles in subjects homozygous and heterozygous for the wildtype intron 2 haplotype, using genomic DNA as internal control for each subject. The results reveal a significant deviation from the expected expression ratio in those heterozygous for the intron 2 haplotype (mean 0.2073, +/- SD 0.0135) when compared with to those without the variant (mean 0.1239, +/- SD 0.0682), p=0.0297 (Fig D).
Conclusion: Intronic variants of PKLR are associated with hospitalization rate for acute pain episodes in adults and children with SCD. We show that the intronic variants are likely to influence acute pain by affecting expression of the PKLR gene using allele-specific expression analyses, although the causal variant is unclear. These results support PKLR as a genetic modifier of SCD.
No relevant conflicts of interest to declare.